- Research
- Open access
- Published:
Critical care nurses’ knowledge and attitudes and their perspectives toward promoting advance directives and end-of-life care
BMC Nursing volume 21, Article number: 278 (2022)
Abstract
Background
End-of-life care can be a difficult and challenging process for critical care nurses in intensive care units (ICUs) due to the care plan shifts from providing life-sustaining measures to end-of-life care. The aims of this study were to assess critical care nurses' perceived knowledge and attitudes toward end-of-life care, as well as their perspectives on promoting advance directives and the associated factors.
Methods
A cross-sectional study was undertaken in an acute major metropolitan medical center in northern Taiwan between February and March 2020, and 250 critical care nurses were invited to participate in the study. Data on demographics, self-perceived knowledge of end-of-life care, attitudes toward end-of-life care, and perspectives of promoting advance directives were collected. A multiple linear regression model with stepwise selection was used to identify factors associated with their perspectives of promoting advance directives.
Results
The law related to end-of-life care was rated as the least familiar part of the self-perceived end-of-life care knowledge, while ‘I have sufficient knowledge to care for patients who have accepted end-of-life care’ was the lowest level of agreement in attitude scores among critical care nurses. Increased levels of perceived knowledge (β = 0.134; p = 0.045) and attitudes (β = 0.423; p < 0.001) toward end-of-life care were associated with the perspectives of promoting advance directives. Nurses who worked in cardiac (β = -0.234; p < 0.001) and respiratory ICUs (β = -0.135; p = 0.024) had less motivation to promote advance directives (F = 16.943; p < 0.001).
Conclusion
Given their important contributions to ICU care services, appropriate and meaningful support is required to optimize critical care nurses' involvement in end-of-life care. This study demonstrated a significant impact on perspectives of promoting advance directives of critical care nurse participants. Findings from this study can inform the design of effective nurse support programs to enhance the promotion of advance directives in intensive care settings.
Introduction
In Taiwan, the Hospice Palliative Care Act was enacted into law in 2000, providing patients suffering from a terminal illness who were certified by two physicians the authority to sign advance directives and do not resuscitate (DNR) orders [1]. A directive can be made in one of two ways “(1) it can be signed by a competent terminally ill patient or (2) it can be signed by a surrogate decision-maker, most commonly a close family member when a patient is unable to make such a decision for themselves due to dementia, delirium, or other types of cognitive impairment” [1]. Advance directives are regarded as “a declaration, typically in writing, in which a person stated when mentally competent the type of health care he would desire to have at a future time when he is no longer capable [2].” Advance directives can assist healthcare personnel in respecting and following the preferred treatment of patients [3]. Before deciding on a DNR directive, the physician must consult with the patients and their family members. Initially, this used to exclusively apply to cancer patients in terminal condition, allowing them to receive hospice palliative treatment and make a DNR decision. Later modifications in 2009 increased insurance coverage of hospice and palliative care treatments to include non-malignant terminal conditions such as heart failure, chronic renal failure, liver cirrhosis and severe dementia. One of the most often used advance directives in end-of-life care is that when a person refuses to accept cardiopulmonary resuscitation (CPR) in the case of cardiac or respiratory arrest [1].
End-of-life care can be a difficult and challenging process in an intensive care unit (ICU) because many terminal illnesses involve withholding or withdrawing life-sustaining therapies, and in such situations, the role of critical care nurses shifts from providing life-sustaining measures to end-of-life care [4, 5]. Critical care nurses face these terminal illnesses and provide direct care to critically ill patients in the ICU, and they are in the best position to promote advance directives and provide end-of-life care. However, a study in Taiwan discovered that critical care nurses have significantly lower knowledge of and attitudes toward advance directives than ICU physicians. Also, a disagreement about end-of-life decision-making between ICU physician and nurses was found regarding who initiated conversation about end-of-life care discussion [6]. Insufficient knowledge and low awareness of advance directives are likely to be the reasons that result in challenges for critical care nurses to provide end-of-life care in ICUs [7]. Given the importance of the involvement of critical care nurses in end-of-life care such as decision-making and promoting advance directives, more strategies for practice development to prepare and support nurses in providing end-of-life care in intensive care settings are needed [6, 8]. Understanding the perceived knowledge of and attitudes toward end-of-life care can inform further development of strategies to support nurses in providing end-of-life care and promoting advance directives. Thus, this study aimed to assess (1) critical care nurses' self-perceived end-of-life care knowledge and attitudes toward terminal patients, as well as their perspectives of promoting advance directives; and (2) the factors associated with critical care nurses’ perspectives of promoting advance directives.
Methods
Research design and setting
A cross-sectional survey was conducted among critical care nurses between February and March 2020. The research site was a major acute-care metropolitan medical center with approximately 120 ICU beds located in northern Taiwan.
Participants
Critical care nurses who met the selection criteria were invited to participate in this study. The inclusion criteria were a status as a registered nurse working in an ICU and agreed to participate in this study. Nurses who were receiving a temporary ICU training in the ICU were excluded. Critical care nurses who worked in a pediatric or neonatal ICU or the emergency room were also excluded, given the nature of nursing practice and workload, admitted patients, and the equipment/medications used in between adult ICU, pediatric or neonatal ICU, and the emergency room were different in Taiwan. G* power vers. 3.0.10 software was used to estimate the sample size [9]. The statistical test and model settings for the sample size estimation were as follow: F test as the test family; linear multiple regression: fixed model; R2 deviation from zero as the statistical test with a prior power analysis (given α, power, and effect size); and parameter settings (α = 0.05, 1–β = 0.95. f2 effect size = 0.08, and number of predictors = 3). Parameter settings were established according to a previous study on perspectives of promoting advance directives as an outcome [10]. An estimated sample size of 219 participants was considered sufficient.
Ethical approval
The study protocol was reviewed and approved by the Hospital Institutional Review Board of the research site. Ethical approval was granted with approval no.: 108152-F. Written consent was obtained prior to the commencement of data collection. Subjects who were invited to participate could choose to discontinue their participation at any time.
Data collection
A survey was developed based on a literature review and expert input. The tool was comprised of four parts that had to be completed, namely demographics, self-perceived knowledge of end-of-life care, attitudes toward end-of-life care, and perspectives of promoting advance directives. The survey was distributed by a research assistant to potential participants in person who agreed to join the study.
Demographic characteristics
Information of critical care nurses we collected included gender, age, educational level, years working as an ICU nurse, type of their workplace ICU, and continuing education in end-of-life care per year (hours).
Self-perceived end-of-life care knowledge of terminal patients
In total, 23 questions and a five-point Likert scale were used. Positively keyed questions were assigned 5 as “very familiar”, 4 as “familiar”, 3 as “neither familiar nor unfamiliar”, 2 as “unfamiliar”, or 1 as “very unfamiliar”. The higher the score, the higher the degree of self-perceived end-of-life care knowledge of critical care nurses, and the higher the tendency that critical care nurses would provide end-of-life care. This scale was developed to examine self-perceived end-of-life care knowledge towards terminal patients among critical care nurses. The content validity and the internal consistency (Cronbach’s alpha = 0.94) were established [11].
End-of-life care attitudes towards terminal patients
In total, 17 questions and a five-point Likert scale were adopted, with 5 as “extremely agree”, 4 as “agree”, 3 as “neither agree nor disagree”, 2 as “disagree”, or 1 as “extremely disagree”. The higher the score, the more positive care attitudes towards terminal patients from critical care nurses, and the higher the tendency that the critical care nurses would provide end-of-life care. This scale aimed to assess end-of-life care attitudes among critical care nurses towards terminal patients. The content validity and the internal consistency (Cronbach’s alpha = 0.85) were confirmed [11].
Perspectives of promoting advance directives
Perspectives of promoting advance directives scale were adopted from Hsieh et al. (2010) who developed a test for Taiwanese nursing staff. In total, 24 questions with a five-point Likert scale were used, with 1 as “extremely disagree”, 2 as “disagree”, 3 as “neither agree nor disagree”, 4 as “agree”, and 5 as “extremely agree”. Negatively keyed questions were inversely scored when summary scores were computed. The total score of the questionnaire ranged 24 ~ 120 points. The higher the score, the more-positive attitudes nursing staff had towards promoting advance directives. A lower score indicated that there would be challenges or negative attitudes towards discussing advance directives between nursing staff and patients. The content validity and internal consistency (Cronbach’s alpha = 0.80) were confirmed [10].
Data analysis
All data were entered into SPSS© vers. 25.0 for analysis (IBM SPSS Statistics for Windows, vers. 25.0. IBM, Armonk, NY, USA). Descriptive analyses, including the mean, standard deviation (SD), and frequency distributions were used to summarize data relating to demographics, self-perceived knowledge of end-of-life care, attitudes toward end-of-life care, and perspectives of promoting advance directives. Multiple imputation was employed to handle missing values. A multiple linear regression model with stepwise selection was used to identify factors associated with perspectives of promoting advance directives. All variables including demographics were entered in the regression model, and significant variables were selected and included in the final model. The variance inflation factor (VIF) was also examined to discover potential multicollinearity issues between variables. Statistical significance for all tests was set to p < 0.05.
Results
Participants
In total, 250 responses were received. Of these, 88.4% (n = 220) of subjects were female, and 76.0% (n = 341) were aged 20 ~ 30 years (Table 1). Ninety-two percent (n = 231) of participants had an undergraduate education level, and more than half (n = 148; 59.2%) had been an ICU nurse for 1 ~ 5 years. Most (n = 76; 30.4%) participants worked in a medical ICU, followed by surgical ICUs (n = 57; 22.8%) and cardiac ICUs (n = 54; 21.6%). Almost all participants (n = 244; 98.0%) received ≤ 5 h of continuing education in end-of-life care per year.
Self-perceived end-of-life care knowledge of and attitudes towards terminal patients
Critical care nurses reported that ‘I am familiar with the importance of collaboration among end-of-life care team members’ (mean = 4.17; SD = 0.54), ‘I am familiar with the purpose of end-of-life care’ (mean = 4.12; SD = 0.51), and ‘I am familiar with the role and function of an end-of-life care team member’ (mean = 4.12; SD = 0.53) were the most familiar self-perceived aspects of end-of-life care knowledge towards terminal patients, demonstrating higher degree of self-perceived end-of-life care knowledge than other items. The least familiar part of the self-perceived end-of-life care knowledge with the lowest score was ‘I am familiar with the laws relating to end-of-life care’ (mean = 3.42; SD = 0.92), showing that the nurses had lower degree of self-perceived end-of-life care knowledge regarding the laws relating to end-of life care (Table 2). As for the end-of-life care attitudes of critical care nurses towards terminal patients, ‘I believe that providing end-of-life care information to patients and their family is beneficial’ (mean = 4.40; SD = 0.57), ‘I will agree to disconnect the ventilator under legal conditions for a terminal patient’ (mean = 4.38; SD = 0.58), and ‘I believe that high-quality end-of-life care can reduce medical disputes’ (mean = 4.34; SD = 0.62) were the most familiar items, while ‘I have sufficient knowledge to care for patients who have accepted end-of-life care’ was the item with the lowest level of agreement in attitude scores (Table 3).
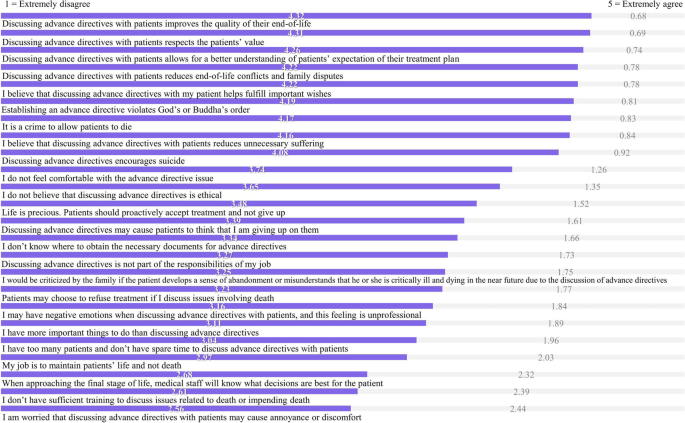
Critical care nurses’ perspectives of promoting advance directives
Figure 1 shows that statements with higher agreement of perspectives of promoting advance directives were ‘Discussing advance directives with patients improves the quality of their end-of-life’ (mean = 4.32; SD = 0.53), ‘Discussing advance directives with patients respects patients’ values’ (mean = 4.31; SD = 0.52), and ‘Discussing advance directives with patients allows for a better understanding of patients’ expectations of their treatment plans (mean = 4.26; SD = 0.54)’, and the statement with the lowest agreement was ‘I am worried that discussing advance directives with patients may cause annoyance or discomfort’ (mean = 2.56; SD = 1.01).
Statements of perspectives of promoting advance directives among critical care nurses. Note. Ordered by mean values, the higher the score, the more-positive attitude critical care nurses had towards promoting advance directives. A lower score (1 or 2) indicates that there would be challenges or negative attitudes towards discussing advance directives between critical care nurses and patients
Factors associated with perspectives of promoting advance directives
The stepwise multiple regression analysis revealed that critical care nurses self-perceived end-of-life care knowledge (β = 0.134; p = 0.045) and attitudes (β = 0.423; p < 0.001) towards terminal patients were factors associated with perspectives of promoting advance directives. Nurses with higher self-perceived end-of-life care knowledge and more-positive end-of-life care attitudes had higher motivation to promote advance directives. Also, compared to nurses who worked in medical ICUs, those who worked in cardiac (β = -0.234; p < 0.001) and respiratory (β = -0.135; p = 0.024) ICUs had lower motivation to promote advance directives (F = 16.943; p < 0.001). All VIFs were < 10 which showed that no multicollinearity issue existed in the regression model (Table 4).
Discussion
This study assessed critical care nurses' self-perceived knowledge of and attitudes toward end-of-life care, as well as their perspectives of promoting advance directives. Critical care nurses demonstrated high perceived knowledge of end-of-life care on items about the purpose of end-of-life care, the role and function of end-of-life care team members, and the importance of collaboration among end-of-life care team members. This shows that critical care nurses are equipped with fundamental knowledge of end-of-life care and understand that teamwork with other healthcare professionals in the end-of-life care team is important. Other research suggested that interprofessional interventions and interdisciplinary teamwork have the potential to support ICU staff to provide better end-of-life care [12,13,14]. The least familiar item among critical care nurses was about laws relating to end-of-life care, which referred to the Hospice Palliative Care Act in Taiwan [1]. Future studies, interventions, and continuing education can consider putting more efforts in enhancing critical care nurses’ understanding of end-of-life care law.
In line with previous studies that attitudes toward end-of-life in critical care nurses are positive [6, 7, 11], both self-perceived knowledge of and attitudes toward end-of-life care were found to be significant factors of perspectives of promoting advance directives, and future studies can be informed by our findings to develop tailor-made interventions for getting critical care nurses involved and engaged in end-of-life care and decision-making processes [15]. The role of critical care nurses being actively involved in end-of-life care and discussions has been highlighted, and they are essential partners in the end-of-life decision-making process within the end-of-life care team [16]. Increasing nurses’ knowledge and confidence to provide input in end-of-life discussions needs more research attention [17, 18].
Our findings also revealed that critical care nurses realized that discussing advance directives with patients improved their quality of end-of-life, respected their values, and allowed for a better understanding of patients’ expectations of their treatment plans. In addition, critical care nurses were not worried that discussing advance directives with patients might cause annoyance or discomfort. This is dissimilar to a previous study that assessed perspectives of promoting advance directives among nurses working in a hemodialysis room, in which more than 65% of those nurses were worried that discussing advance directives with patients might cause annoyance or discomfort [10]. A possible reason might be that as critical care nurses are frontline care providers who care for critically ill patients, they understand that advance directives would be one of the options to provide better end-of-life care and they have to face many patients with terminal illnesses and dying patients [19, 20]. Also, we identified that compared to nurses who work in medical ICUs, those who work in cardiac and respiratory ICUs have lower motivation to promote advance directives. This is likely because mortality rates in and the severity of diseases are higher in medical ICUs in Taiwan. We suggest adding advance directives-relevant information on laws into the content of continuing education for end-of-life care, particularly for cardiac and respiratory ICU nurses. Educational strategies such as simulated education with role-playing scenarios to introduce advance directives to patients would likely be effective in improving nurses’ end-of-life care [21, 22]. Furthermore, the dignity of patients with palliative needs were also needed to be considered when developing the aforementioned educational strategies for nurses to promote palliative care. As a comprehensive integrated review has summarized a model of dignity that identifying several themes such as family care and support, social justice, reliable health care, which are highly relevant to be embedded in providing nursing care [23].
Study limitations
The main limitation of this study to be acknowledged is that the survey was only distributed to participants in a major acute-care metropolitan medical center located in northern Taiwan. The nonprobability sampling method used in this study to choose the hospital may influence the external validity of the study, and therefore, the results may not be generalizable to other areas in Taiwan due to representative bias. Future research should enroll more participants that particularly reflect different areas to conduct a multicenter study to compare the results. Nevertheless, this study discovered critical care nurses' perceived knowledge and attitudes toward end-of-life care, as well as their perspectives on promoting advance directives and the associated factors using validated instruments. Findings from this study can inform the design of effective nurse support programs to enhance the promotion of advance directives in intensive care settings.
Conclusions
Self-perceived knowledge and attitudes toward end-of-life care, and perspectives of promoting advance directives of critical care nurses were assessed. We found that increased levels of perceived knowledge and attitudes toward end-of-life care were associated with the perspectives of promoting advance directives. Nurses who worked in cardiac and respiratory ICUs had less motivation to promote advance directives. This study demonstrated a significant impact of perspectives of promoting advance directives of critical care nurse participants. Given their important contribution to ICU care services, appropriate and meaningful support is required to optimize critical care nurses' involvement in end-of-life care.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Hospice palliative care act. Available from: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=L0020066. Accessed 30 Sep 2022.
Introduction of the concept of advance directives in Hong Kong. Available from: https://www.gov.hk/en/residents/government/publication/consultation/docs/2010/AdvanceDirectives.pdf. Accessed 30 Sep 2022.
Ford DW, Koch KA, Ray DE, Selecky PA. Palliative and end-of-life care in lung cancer: diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e498S-e512S.
Ozga D, Woźniak K, Gurowiec PJ. Difficulties perceived by ICU nurses providing end-of-life care: a qualitative study. Glob Adv Health Med. 2020;9:2164956120916176.
Kisorio LC, Langley GC. Intensive care nurses’ experiences of end-of-life care. Intensive Crit Care Nurs. 2016;33:30–8.
Ke YX, Hu SH, Takemura N, Lin CC. Perceived quality of palliative care in intensive care units among doctors and nurses in Taiwan. Int J Qual Health Care. 2019;31(10):741–7.
Velasco-Sanz TR, Rayón-Valpuesta E. Advance directives in intensive care: health professional competences. Med Intensiva. 2016;40(3):154–62.
Riegel M, Randall S, Ranse K, Buckley T. Healthcare professionals’ values about and experience with facilitating end-of-life care in the adult intensive care unit. Intensive Crit Care Nurs. 2021;65:103057.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Hsieh LY, Lin SY. A pilot study on the perspectives of hemodialysis room nurses on promoting advance directives. J Nurs. 2010;57(4):59–67.
Su LH, Huang ML, Lin YL, Wu CK, Lin FR, Lin HM, Huang SJ. Knowledge and attitudes of clinical nurses regarding end-of-life care: survey in a regional hospital in central Taiwan. Taiwan J Hosp Palliat Care. 2008;13(4):431–46.
Blythe JA, Kentish-Barnes N, Debue AS, Dohan D, Azoulay E, Covinsky K, Matthews T, Curtis JR, Dzeng E. An interprofessional process for the limitation of life-sustaining treatments at the end of life in France. J Pain Symptom Manage. 2022;63(1):160–70.
Schwarzkopf D, Pausch C, Kortgen A, Guenther A, Reinhart K, Hartog CS. Quality improvement of end-of-life decision-making and communication in the ICU : effect on clinicians’ burnout and relatives’ distress. Med Klin Intensivmed Notfmed. 2020;115(7):600–8.
Graham R, Lepage C, Boitor M, Petizian S, Fillion L, Gélinas C. Acceptability and feasibility of an interprofessional end-of-life/palliative care educational intervention in the intensive care unit: a mixed-methods study. Intensive Crit Care Nurs. 2018;48:75–84.
Badır A, Topçu İ, Türkmen E, Göktepe N, Miral M, Ersoy N, Akın E. Turkish critical care nurses’ views on end-of-life decision making and practices. Nurs Crit Care. 2016;21(6):334–42.
Benbenishty J, Ganz FD, Anstey MH, Barbosa-Camacho FJ, Bocci MG, Çizmeci EA, Dybwik K, Ingels C, Lautrette A, Miranda-Ackerman RC, et al. Changes in intensive care unit nurse involvement in end of life decision making between 1999 and 2016: Descriptive comparative study. Intensive Crit Care Nurs. 2022;68:103138.
Khater WA, Akhu-Zaheya LM, Al-Nabulsi HW, Shattnawi KK, Shamieh O, Joseph R. Barriers to implementing palliative care in intensive care units: perceptions of physicians and nurses in Jordan. Int J Palliat Nurs. 2021;27(2):98–106.
Henao-Castaño ÁM, Rivera-Romero N, Garzón HPO. Health care at the end of life: experience of nurses at the adult intensive care unit. Crit Care Nurs Q. 2021;44(4):387–92.
Bayuo J, Anago EK, Agyei FB, Salifu Y, Kyei Baffour P, Atta Poku C. “Resuscitate and push”: end-of-life care experiences of healthcare staff in the emergency department - a hermeneutic phenomenological study. J Palliat Care. 2022;37(4):494–502.
Jang SK, Park WH, Kim HI, Chang SO. Exploring nurses’ end-of-life care for dying patients in the ICU using focus group interviews. Intensive Crit Care Nurs. 2019;52:3–8.
Novaes LMS, Paiva E, O’Mahony A, Garcia ACM. Roleplay as an educational strategy in palliative care: a systematic integrative review. Am J Hosp Palliat Care. 2022;39(5):570–80.
Tamaki T, Inumaru A, Yokoi Y, Fujii M, Tomita M, Inoue Y, Kido M, Ohno Y, Tsujikawa M. The effectiveness of end-of-life care simulation in undergraduate nursing education: a randomized controlled trial. Nurse Educ Today. 2019;76:1–7.
Dakessian Sailian S, Salifu Y, Saad R, Preston N. Dignity of patients with palliative needs in the Middle East: an integrative review. BMC Palliat Care. 2021;20(1):112.
Acknowledgements
We would like to thank the critical care nurses who so generously participated in the survey.
Funding
None.
Author information
Authors and Affiliations
Contributions
MHH: design of the work, the acquisition, analysis, interpretation of data, have drafted the work; HCL: analysis, interpretation of data; JYJ: design of the work, interpretation of data; JJL: analysis, interpretation of data, have drafted the work; MFL: design of the work, analysis, interpretation of data, have drafted the work. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Far Eastern Memorial Hospital Research Ethics Review Committee in Taiwan for ethical considerations (approval number: 108152-F). All methods were carried out in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants. Legally Authorized Representatives of illiterate participants provided informed consent for the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ho, MH., Liu, HC., Joo, J.Y. et al. Critical care nurses’ knowledge and attitudes and their perspectives toward promoting advance directives and end-of-life care. BMC Nurs 21, 278 (2022). https://doi.org/10.1186/s12912-022-01066-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-022-01066-y